May 13, 2018
53 days since injury.
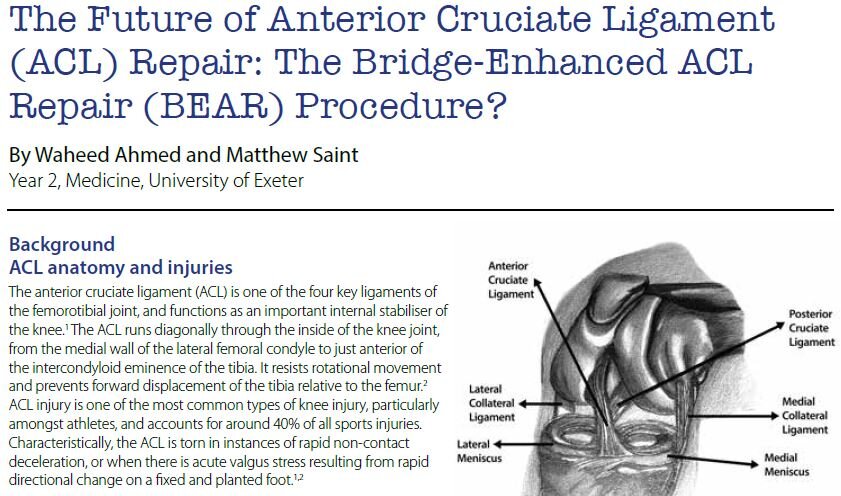
I come across some info on ALL (Anterolateral Ligament) and find:
‘Despite technologic advances in the surgical technique for ACL reconstruction, some patients continue to have rotational instability post operatively, decreasing the return to sport rate. Failures can occur because of improper tunnel positioning, problems with patient rehabilitation, or non-optimal incorporation of the graft used for reconstruction’
and
‘recent biomechanical studies have shown it is an important stabilizer against anterolateral tibial rotation’
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5263705
Then found in Dr DiFelice NY’s article
Ground Breaking ACL Repair Approach Could Help 80,000 in US Alone
“Skier Veronika Velez Zuzulova competed 20 weeks after suffering a torn right ACL: an injury that according to traditional thinking should have required ACL Reconstruction Surgery and an 8 - 12 month #recovery.
Foregoing the traditional, Zuzulova opted for ground breaking ACL repair surgery instead of ACL removal & graft reconstruction – that had her training just 6 weeks after surgery with enough time to enable her to be ready for the Pyeong Chang Olympic Games.”
“more than 150 Repairs and has published both two-year and five-year post-surgery data on his initial cohort to validate the procedure’s success”
“published more than 15 professional, peer-reviewed articles on the subject”
“unwarranted bias which limited ACL Repair as an option”
“failing to recognize that ACL Repair success was much higher when treating specific types of tears, the data lead to the erroneous conclusion that ACL Repair was not a reliable course of action.”
Can “repair greater than 50% of the athletes who present to him with ACL tear”
“up to 80,000 of the 300,000 patients suffering ACL tears in the US alone may be helped”
French surgeon Dr. Bertrand Sonnery Cottet performed Zuzulova’s surgery, and again the article mentioned Scotland's Dr. Gordon MacKay at The Mackay Clinic.